You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Something funny.
- Thread starter JB Cases
- Start date
Yes
It does kind of sum things up doesn't it? I used to be fairly heavily into paintball. One afternoon one of our players slid down a small cliff. After we got him back up several people were all excited running around saying are you alright etc. Tony jumped with a look of concern his eyes, jumped up, turned around and shot a few rounds at a tree, sighed and said yes.
It does kind of sum things up doesn't it? I used to be fairly heavily into paintball. One afternoon one of our players slid down a small cliff. After we got him back up several people were all excited running around saying are you alright etc. Tony jumped with a look of concern his eyes, jumped up, turned around and shot a few rounds at a tree, sighed and said yes.
TheThaiger
Banned
It does kind of sum things up doesn't it?
It does? I don't get it.
Very nice, John. That fellows artwork is first rate. :smile:
It does? I don't get it.
Lol...John, please don't explain it to him. I think if he REALLLLY wants to get it, he will figure it out.
Great artwork. thank God I have a JB Case too.
This idea has been rattling around in my head for about 15 years and Dino drew it for me.
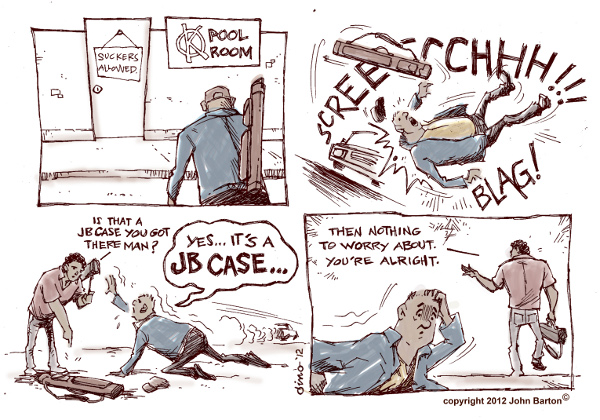
That's a great comic for those in the know! :grin:
It does kind of sum things up doesn't it? I used to be fairly heavily into paintball. One afternoon one of our players slid down a small cliff. After we got him back up several people were all excited running around saying are you alright etc. Tony jumped with a look of concern his eyes, jumped up, turned around and shot a few rounds at a tree, sighed and said yes.
I thought you were going to say he shot all of the enemy combatants..
That's a great comic for those in the know! :grin:
in the know of what???
It does? I don't get it.
That's a great comic for those in the know! :grin:
in the know of what???
"In the know" of what TheThaiger doesn't.
-Sean
Jb cases
John,,
You should put that cartoon on your ''Home Page'' on your website,,
Funny,,,and True,!!
Alan Ende
John,,
You should put that cartoon on your ''Home Page'' on your website,,
Funny,,,and True,!!
Alan Ende
It does? I don't get it.
I'll try to put it in words we can all understand. Between 2% and 4% of the general population suffers chronic widespread pain, accompanied by paresthesias, . These discrepancies may have an essential underlying reason: As physicians and other providers do not have a coherent theoretical framework to accommodate FM. Current linear-reductionist medical paradigm cannot explain this complex disease. 3. Prevailing Medical Paradigm. The prevailing medical paradigm is based on a linear-reductionist algorithm: the clinical–pathological correlation. In this construct, a group of symptoms and signs (the effect) is linearly explained by a discrete anatomical lesion, or an abnormal lab test (the cause). Reductionism proposes that the whole can be understood by analyzing each of its parts. Accordingly, at present, MRIs, biopsies, or blood or other tests are able to explain the cause of nearly all clinical syndromes. Nevertheless, this linear-reductionist model is clearly unable to explain complex illnesses such FM.3 4.Information: Explain complex characteristics of FM. A well-written and well-annotated book is useful in achieving this task. In my experience, most patients agree with the dysautonomia model. Points to highlight to patients are validation of symptoms; explanation of role of genetics and external stressors on the hyperadrenergic state; and explanation of the neuropathic nature of pain. 5golgenrings.Avoidance of sympatho-mimetic substances: These include caffeine and nicotine.6-14 huthut. Biofeedback techniques: Based on electromyography or heart rate variability.7sub chaperS. Cognitive-behavioral therapy and other self-efficacy techniques8. Psychological and psychiatry counseling 8 . Pharmacological therapy: Polypharmacy should be avoided. Drugs that may improve pain include paracetamol, tramadol, antineuropathic agents such as pregabalin and gabapentin, triciclic antidepressants, and tropisetron. Complexity theory.4-6a - c This paradigm derives from cybernetics and computer modeling of natural phenomena, such as weather. 7.1a Such systems are open, elastic, and constantly adapting to the environment through positive and negative feedback loops (complex adaptive systems). The systems have nonlinear behavior; as such, the intensity of the stimulus is dissimilar to the magnitude of the response. These systems cannot be understood by analyzing each of its components individually, because for them, the whole is different than the sum of its parts. Examples of complex adaptive systems include the following: democratic societies, stock markets, ant colonies, and the major systems of the human body. Complex systems have wide varying behaviors. If a system becomes rigid, it ultimately dies. 7.1.a.b The best way to understand complex systems is with viewing the system dynamics in its entirety and observing its interactions with the environment. Complexity theory provides a scientific foundation for holism. Rather than opponents, holism and reductionism should be regarded as complementary scientific tools; both perspectives are needed for a proper account of reality. ons. The main homeostatic systems of the human body are complex. Static blood tests or imaging techniques cannot detect dysfunction of such homeostatic systems. Autonomic Nervous System: Prototype of Complex Adaptive System The best example of a complex adaptive system in the human body is the autonomic nervous system (ANS).7stillgoing The fundamental role of the ANS in health maintenance is represented by the fact that it regulates vital signs. The performance of the ANS cannot be appreciated with linear tools. There is a novel, nonlinear procedure based on computer calculations called heart rate variability analysis. This method demonstrates that young healthy individuals have flexible sympathetic–parasympathetic harmonious interactions. With disease or aging, the system becomes rigid, thus losing its complexity.8OMGWTF In other words, disorder can be healthy while uniformity can lead to disease. Complexity Loss in Fibromyalgia
Several groups of investigators have shown that FM patients have decreased heart rate variability. This alteration can be interpreted as sign of “decomplexification” of the ANS with persistent rigid circadian sympathetic hyperactivity. Rigid sympathetic hyperactivity can lead to aberrant neuroplasticity, establishing abnormal connections between the sympathetic nervous system and the nociceptive system. Animal models have identified the dorsal root ganglia as an important short-circuit site. Triggering events for FM could be physical or emotional trauma as well as different types of infections. The resulting clinical syndrome is a sympathetically maintained neuropathic pain syndrome (pain, allodynia, and paresthesias). Sympathetic hyperactivity may cause other FM symptoms not related to pain. Degraded environment may explain the high prevalence of FM at present. Industrialization has disfigured circadian cues, diets, exercise, and working conditions among many other variables. Susceptible individuals such as women with deficient catecholamine-handling enzymes would be more prone to become ill. FM can therefore be viewed as a failed attempt of our main complex system to adapt to a hostile environment.
Of course, much more research is needed to confirm or amend this model.
Last edited:
This idea has been rattling around in my head for about 15 years and Dino drew it for me.
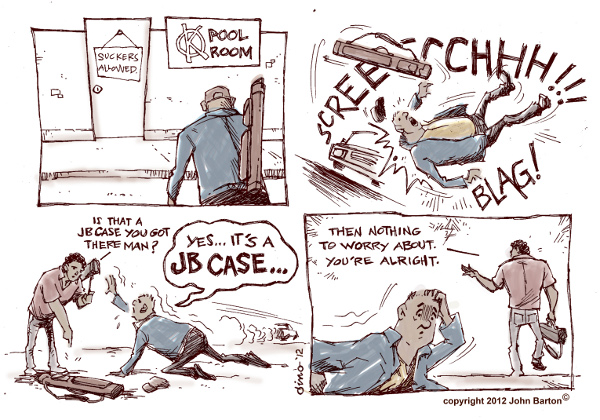
I like it, very professional. Who is Dino and is he a cartoonist for a living?
Excellent, John.
I remember when we used one of your cases behind a tire to keep the huge trailer full of cases and fixtures from rolling down the highway so you can take the car to get a cotter pin. It was loaded with cues that were totally unharmed.
You make one tough case!
Dave
I remember when we used one of your cases behind a tire to keep the huge trailer full of cases and fixtures from rolling down the highway so you can take the car to get a cotter pin. It was loaded with cues that were totally unharmed.
You make one tough case!
Dave
TheThaiger
Banned
I'll try to put it in words we can all understand. Between 2% and 4% of the general population suffers chronic widespread pain, accompanied by paresthesias, . These discrepancies may have an essential underlying reason: As physicians and other providers do not have a coherent theoretical framework to accommodate FM. Current linear-reductionist medical paradigm cannot explain this complex disease. 3. Prevailing Medical Paradigm. The prevailing medical paradigm is based on a linear-reductionist algorithm: the clinical–pathological correlation. In this construct, a group of symptoms and signs (the effect) is linearly explained by a discrete anatomical lesion, or an abnormal lab test (the cause). Reductionism proposes that the whole can be understood by analyzing each of its parts. Accordingly, at present, MRIs, biopsies, or blood or other tests are able to explain the cause of nearly all clinical syndromes. Nevertheless, this linear-reductionist model is clearly unable to explain complex illnesses such FM.3 4.Information: Explain complex characteristics of FM. A well-written and well-annotated book is useful in achieving this task. In my experience, most patients agree with the dysautonomia model. Points to highlight to patients are validation of symptoms; explanation of role of genetics and external stressors on the hyperadrenergic state; and explanation of the neuropathic nature of pain. 5golgenrings.Avoidance of sympatho-mimetic substances: These include caffeine and nicotine.6-14 huthut. Biofeedback techniques: Based on electromyography or heart rate variability.7sub chaperS. Cognitive-behavioral therapy and other self-efficacy techniques8. Psychological and psychiatry counseling 8 . Pharmacological therapy: Polypharmacy should be avoided. Drugs that may improve pain include paracetamol, tramadol, antineuropathic agents such as pregabalin and gabapentin, triciclic antidepressants, and tropisetron. Complexity theory.4-6a - c This paradigm derives from cybernetics and computer modeling of natural phenomena, such as weather. 7.1a Such systems are open, elastic, and constantly adapting to the environment through positive and negative feedback loops (complex adaptive systems). The systems have nonlinear behavior; as such, the intensity of the stimulus is dissimilar to the magnitude of the response. These systems cannot be understood by analyzing each of its components individually, because for them, the whole is different than the sum of its parts. Examples of complex adaptive systems include the following: democratic societies, stock markets, ant colonies, and the major systems of the human body. Complex systems have wide varying behaviors. If a system becomes rigid, it ultimately dies. 7.1.a.b The best way to understand complex systems is with viewing the system dynamics in its entirety and observing its interactions with the environment. Complexity theory provides a scientific foundation for holism. Rather than opponents, holism and reductionism should be regarded as complementary scientific tools; both perspectives are needed for a proper account of reality. ons. The main homeostatic systems of the human body are complex. Static blood tests or imaging techniques cannot detect dysfunction of such homeostatic systems. Autonomic Nervous System: Prototype of Complex Adaptive System The best example of a complex adaptive system in the human body is the autonomic nervous system (ANS).7stillgoing The fundamental role of the ANS in health maintenance is represented by the fact that it regulates vital signs. The performance of the ANS cannot be appreciated with linear tools. There is a novel, nonlinear procedure based on computer calculations called heart rate variability analysis. This method demonstrates that young healthy individuals have flexible sympathetic–parasympathetic harmonious interactions. With disease or aging, the system becomes rigid, thus losing its complexity.8OMGWTF In other words, disorder can be healthy while uniformity can lead to disease. Complexity Loss in Fibromyalgia
Several groups of investigators have shown that FM patients have decreased heart rate variability. This alteration can be interpreted as sign of “decomplexification” of the ANS with persistent rigid circadian sympathetic hyperactivity. Rigid sympathetic hyperactivity can lead to aberrant neuroplasticity, establishing abnormal connections between the sympathetic nervous system and the nociceptive system. Animal models have identified the dorsal root ganglia as an important short-circuit site. Triggering events for FM could be physical or emotional trauma as well as different types of infections. The resulting clinical syndrome is a sympathetically maintained neuropathic pain syndrome (pain, allodynia, and paresthesias). Sympathetic hyperactivity may cause other FM symptoms not related to pain. Degraded environment may explain the high prevalence of FM at present. Industrialization has disfigured circadian cues, diets, exercise, and working conditions among many other variables. Susceptible individuals such as women with deficient catecholamine-handling enzymes would be more prone to become ill. FM can therefore be viewed as a failed attempt of our main complex system to adapt to a hostile environment.
Of course, much more research is needed to confirm or amend this model.
Ah, thanks - much clearer. Actually, I was just baiting Barton. He's not biting to anything these days, so now I'm getting genuinely worried. Someone has him and is doing him terrible harm, presumably. Either that or some sort of revolutionary personality transplant. These Chinese are fiendishly clever.
BRING BACK BARTON!